DEMOGRAPHICS
Name: L.A.
Age: 49 years old
Case/Type: Medium/Type II
ASSESSMENT
This patient had her last medical exam in March of 2019. She doesn’t have any allergies but she does have iron-deficiency anemia and manages it through diet and by taking a daily OTC iron supplement.
L.A.’s blood pressure reading was 106/72 and her pulse was 65 beats per minute.
L.A. does not drink alcohol or smoke.
L.A. did not require any premedication for dental treatment.
L.A. takes an OTC iron supplement (65 mg, two times per day).
ORAL PATHOLOGY (Extraoral and Intraoral findings)
L.A.’s extraoral exam produced bilateral submandibular swelling. She did not report any pain. A leukoedema was found on the patient’s lower right side along with a coated, slightly scalloped tongue. L.A. also exhibited signs of experiencing chemical burn on her lower lip due to Listerine Antiseptic use.
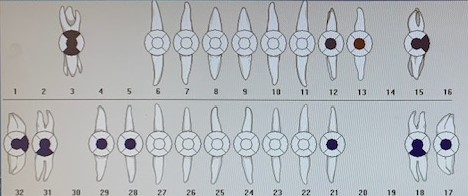
DENTITION
L.A.’s class of occlusion was Class I with 50% overbite and 3 mm overjet.
L.A. was missing teeth #s 1, 2, 16 and 17. Teeth #s 6-11 and 22-27 had mild attrition. Teeth #s 6-11 also exhibited incisal erosion.
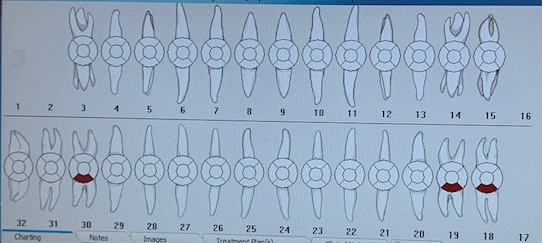
L.A. had caries present on teeth #s 18B, 19B and 30B
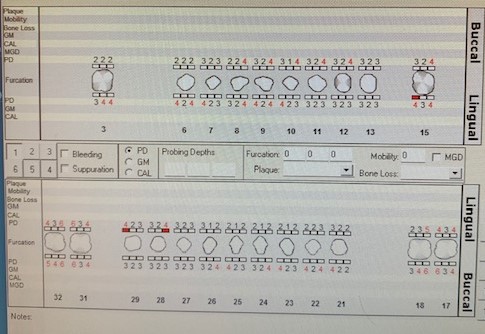
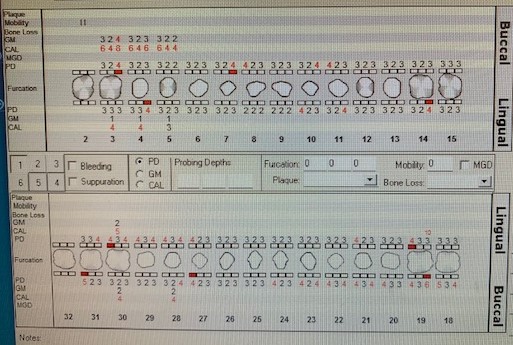
PERIODONTAL
L.A. was classified as a Medium Case, Type II. This patient’s probing depths were between 3-5 mm. She had minimal bleeding upon probing. L.A. also had generalized recession 2-3 mm.
ORAL HYGIENE
L.A.’s initial plaque score was 1.3 (fair). At the time of her subsequent appointment, the plaque index score was 1.0 (fair).
L.A. had generalized light staining and generalized moderate interproximal subgingival calculus deposits.
L.A. reported brushing two times per day with an electric toothbrush. She also stated that he flosses once per day with traditional waxed dental floss and rinses once per day with Listerine Total Care mouthwash and coconut oil (“oil-pulling”). L.A. reported using non-fluoridated toothpaste such as “Desert Essence.” I reviewed the appropriate electric toothbrushing technique with this patient (she was using it like a manual toothbrush). I also recommended that the patient use fluoridated toothpaste.
At the patient’s next visit, I demonstrated flossing with waxed dental floss and the patient practiced the technique.
RADIOGRAPHS
L.A. had an FMS done at a private dental practice in July of 2017. She required two periapical radiographs of teeth #s 18, 19, 30 and 31 to assess the level of bone loss in the intended Arestin placement sites.


ARESTIN PLACEMENT
I placed Arestin (minocycline HCl microspheres 1 mg) in the following sites: #18MB, #19DB, #30DL and #31DB on April 15th, 2019.
*L.A. refused before and after intraoral photos.
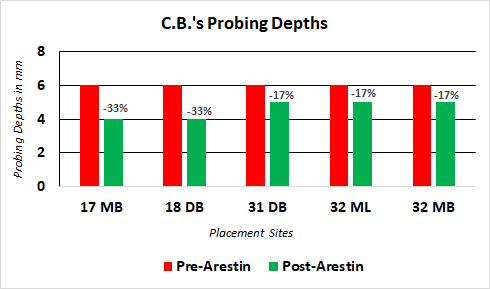
ARESTIN EVALUATION
L.A. returned for a post-Arestin placement evaluation on May 16th, 2019. The following graph shows the reduction in pocket depths in the sites that were treated with Arestin.
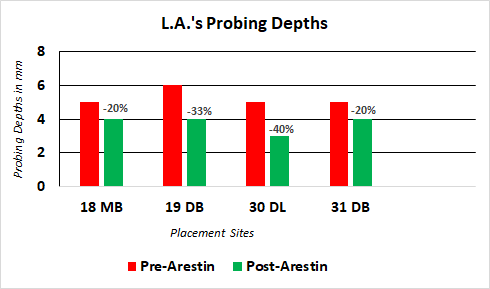
A