Case Study 1:
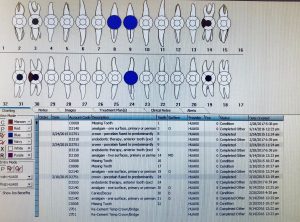
J.V., Male, 48 years old, Heavy/ Periodontal type IV. ASA I. Vital Signs: BP 143/103 P 85. (Second reading 141/90). Hispanic patient with no medical conditions, no allergies and taking no medications. Past history of smoking, severe alcoholism, induced vomiting and acid reflux. Severe dental erosion due to habit of sucking on lemons, constant alcohol consumption, and chewing on chiles 3 times per week. Fractured anterior teeth due to habit of opening beer bottles with his teeth and severe bleeding upon probing and bulbous tissue along the posterior teeth.
Patient presented with decay on the occlusal surfaces of #14, #17, #18, #19, #20. Amalgams on the distal of #21 and the mesial of #20. FMS was exposed, the findings included generalized moderate horizontal bone loss with localized vertical bone loss and decay on #2, #11, #21, #22, #27, #28, #30, #31 and #32. Referral was dispensed to patient for decay and periodontal disease. Patient refused to complete cleaning reporting he experienced severe pain and dental anxiety.
Case Study 2:
A. M., Female, 42 years old (Heavy/Periodontal Type 2) ASA II. Vital Signs: BP 123/81 P 64. Depression and Medication Induced Xerostomia. Medications: OTC Vitamin B12 daily and Paxil 10mg daily for depression. Patient reported flossing 1x per week, never using an oral rinse and brushing once a day using Colgate toothpaste.
Patient presented with light staining and generalized sub gingival and supra gingival calculus with visible biofilm on direct teeth surfaces. Dental: Occlusal composites (#14, #15, #30). Buccal-Occlusal amalgams (#18, #31) and Occlusal amalgam on #19. Periodontal: Generalized 2-3mm pocket depths with localized 4-7mm pocket depths. Gingival tissue was edematous marginally, erythematous and retractable on the mandibular anteriors with moderate bleeding upon probing. No radiographs were exposed to confirm the evidence of bone loss. Patient exhibited bilateral TMJ crepitation due to bruxism induced from the psychological distress that the patient feels from the depression.
Due to the patients depression she stated the lack of motivation and lack of care for oral hygiene. Patient stated waking up on some days and not brushing due to not feeling enough energy to do so. The antidepressant the patient takes also reduces her salivary flow placing her at a high risk for potential decay. This patient was challenging to treat because she lacked any innate motivation or personal interest towards her oral hygiene. It was difficult to provide treatment as well due to her TMD pain. During debridement we took constant breaks to allow the patient to relax the jaw and we spoke about her life and any interests the patient may have, in order to spark and establish trust between patient-student hygienist.
Recommendations: OTC fluoride containing toothpaste to be used twice daily, biotene gel and 0.05% Sodium Fluoride rinse daily. Also recommended at the best of patients ability to brush twice and introduce the usage of a soft pick 4x per week. This patient was placed on a 3 month recall.
Case Study 3: Arestin Patient
S. Y., 37 year old Caucasian male (Heavy/Periodontal Type 2) ASA I. Vital Signs: BP 111/83 P 76. Patient that has no medical conditions, takes no medications and has no allergies.
Dental: Missing teeth (#1, #16, #17, #32). Occlusal amalgams (#3, #19, #30, #31). Crown with endodontic therapy (#8, #9, #24). Mesio-occusal amalgam on #14. Decay present on the Distal surface of #30.
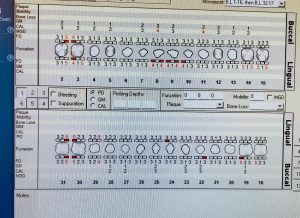
Periodontal: Patient exhibited generalized moderate marginal inflammation. The patients gingiva was erythematous and exhibited generalized biofilm accumulation in the cervical 1/3 of the tooth surfaces. Patient exhibited localized areas of moderate bleeding upon probing. Patient presented with enough calculus presence to be categorized as a heavy. Generalized 1-3mm probing depths with localized 4-5mm pockets were present as well as a suspicious lesion on the occlusal surface of #15. Localized areas ranging with 1-3mm of recession.
(4-5mm pockets in red)
Visit 1: Assessments were completed and vitals were taken. Plaque Score: 1.0. OHI- Recommendation of flossing daily, brushing 2x per day with a soft toothbrush and rinsing with Listerine Antiseptic (10ml for 30 secs) daily. Patient qualified for Arestin (which was placed on the third visit). Debridement of the UR quadrant using ultrasonic and hand scalers.
Visit 2: Digital FMS was available from 02/2016. Due to the time span, to view any changes, suspicious lesions and the bone level, 4BWS were exposed. Radiographic findings exhibited decay present on the distal of #30. Reevaluation of the quadrant previously scaled for residual deposits and tissue response to treatment. Tissue responded well to treatment and showed a decrease in inflammation. Plaque Score showed improvement from 1.0 to 0.7. OHI- Reviewed the way patient has been flossing. Debridement of LR, UL and LL quadrants using ultrasonic and hand scalers. Engine polished using fine paste and application of 5% Fluoride Varnish treatment.
Visit 3: Reevaluation of all quadrants that were scaled to check the tissue response. Patient responded positively to treatment interventions and the tissue showed an increase in resilience and a decrease in bleeding upon probing and inflammation. Patient stated incorporating the OHI recommendations to the best of his abilities. Arestin was placed on six sites #2 DB[7mm], #3 DB[6mm], #30 DL[5mm], #14 ML[5mm], #15 DL[5mm] and #14 DL [5mm]. Verbal post instructions and written post instructions for Arestin placement were dispensed to patient.
Visit 4: Reevaluation of the areas where Arestin was placed. The patients tissue responded well to the Arestin placement for the most part and certain pocket depths showed a great reduction. The patients gingiva was snug to the tooth with no bleeding upon probing and presence of resilience and stippling. Patient presented with a pocket reduction of 2mm on half of the pockets where Arestin had been placed. #3 DB reduced from 6mm to 4mm, #15 DL and #30 DL reduced from 5mm to 3mm. However, #2 DB, #14 ML and DL exhibited no pocket reduction. Patient was placed on a 3 month recall.
The patient was very pleased with the results and expressed the desire to have more Arestin placed in the near future.