Case 1:
21 yr old Middle Eastern male presents for prophylaxis and dental check-up. His vitals were BP: 132/78 P:71 which makes him prehypertensive. No systemic conditions are present in this patient and he isn’t taking any prescription or over the counter medications. He is classified as ASA II based on this information.
The class of occlusion for this patient is class III on the right side and class I on the left. Also, cross bite on anteriors, under bite 20%, and 1 mm over jet. He has severe mandibular anterior crowding, moderate maxillary anterior crowding, a supernumerary tooth distal to #1, and mesially impacted #17. There is recurrent decay on #14 mesial this is a class II classification of caries. This patient has high caries risk level based on the caries risk assessment.
The gingiva is generalized erythematous around the margins, with severe localized marginal inflammation at # 9 and 11, shiny, firm, and knife-edged papillae. Patient has moderate generalized gingivitis. The periodontal findings include generalized 1-3 mm probing depths, localized 4-5 mm pockets posteriorly, moderate bleeding upon probing, and clinical attachment loss as evidenced by localized recession on canines. In addition, this patient is generalized type I periodontitis with localized type II as evidenced by the probing depths and moderate bleeding upon probing. For his plaque score on the first visit, it was a 1.0. The second visit, it remained unchanged.
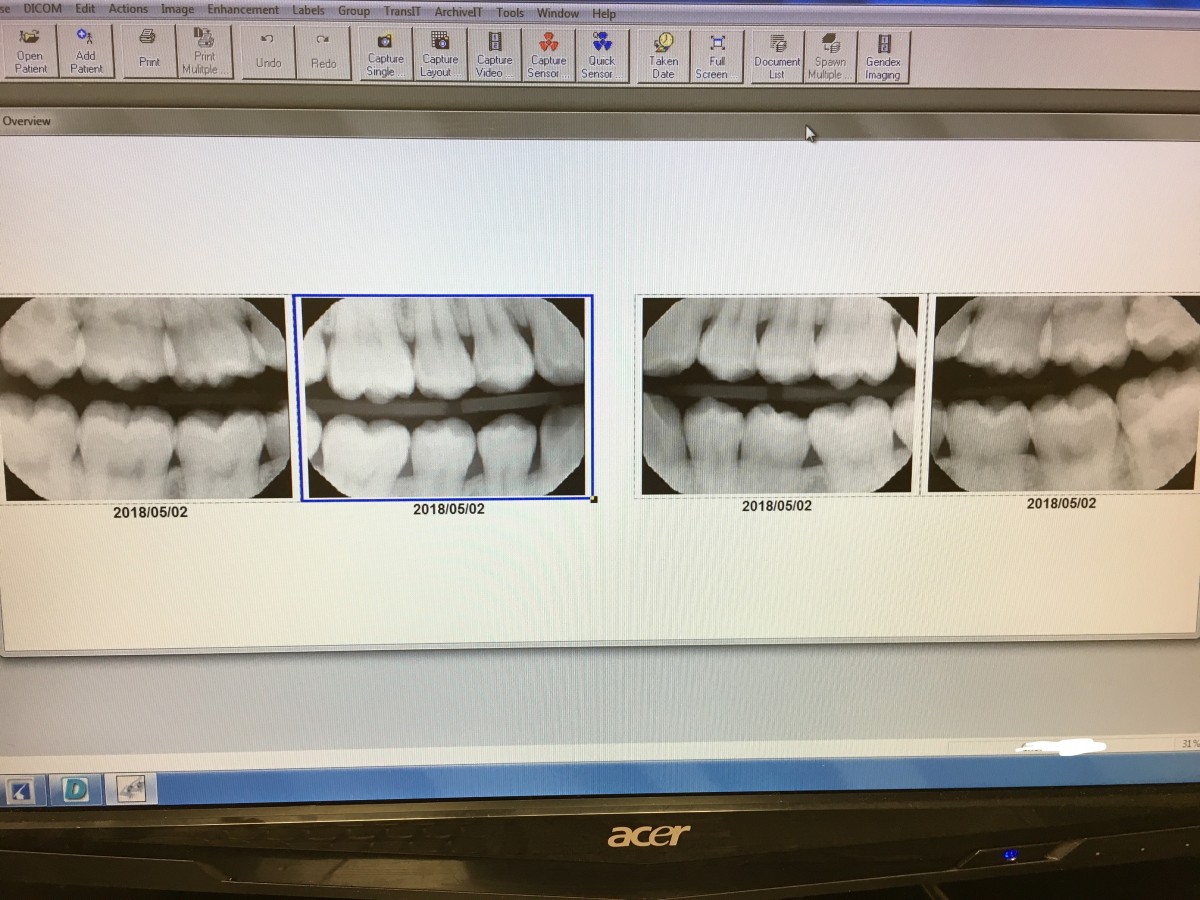
The patient required a panorex and 4 BWs due to missing #1 and after the panorex was taken, recurrent decay on #14 and impacted #1 was revealed in the x-ray. Therefore, to get a better diagnostic x-ray of #14, BWs are required. The BWs confirmed the decay on #14. Two interesting findings that the panorex revealed was a supernumerary tooth distal to #1 and a mesially impacted #17. The were no other factors that might affect the patient’s optimal health. His mandibular anterior crowding is very severe that # 26 was behind #27 and #25 which will be challenging to remove plaque in that area.
For oral hygiene instructions, I originally taught him the modified Bass toothbrushing technique, but during his second visit, I couldn’t see a difference in the plaque score and tissue response to exploring. Therefore, I recommended a power toothbrush because it is more effective in plaque removal according to studies. Also, using an interdental pick for the area around #26 was recommended. As for flossing, I recommended and demonstrated Oral-B Glide wax floss which is perfect for sliding into tight contacts to clean out interproximal plaque. In addition, I recommended Listerine Total mouth rinse twice a day to support enamel remineralization and caries prevention. The patient was compliant with the recommended home care regimen and is motivated to improve his oral health. Referral to an orthodontist and D.D.S. was given for the malocclusion and recurrent decay on #14 respectively. Recare for this patient is 6 months.
I choose this case to present because it was challenging to scale with severely overcrowded teeth especially on #25-27 where there was calculus build-up. Aside from overcrowding, this patient has a history of caries and recurrent decay. I provided some intervention strategies to prevent future decay by conducting a caries risk assessment, recommending a power toothbrush, Glide wax floss, interdental pick, and Listerine Total mouth rinse. Due to his crowding and malocclusion, I had to be creative and modify the oral hygiene instructions in order for the patient to achieve optimum oral health.
Case 2:
The BWS showed healthy bone level and no interproximal caries.
Panorex shows rotated mesiodens between the maxillary centrals and partially erupted #32.
19 yr old Middle Eastern male presents for dental check-up and prophylaxis. Patient’s vitals were BP: 130/80 P: 90 which places him at ASA II. The extraoral/ intraoral exam is WNL. Dentition wise, he has class of occlusion I bilateral, 50% overbite, 8 mm overjet. Demineralization on the buccal surfaces of maxillary canines/ bicuspids along with clinically noticeable caries on #30 occlusal. The gingiva is generalized inflamed and erythematous with localized bulbous margins on anteriors. He also has very sensitive gums on lingual surfaces. Periodontally, he presents as a type I with generalized 3-4 mm PD with moderate BUP. This patient had generalized biofilm on his anteriors and gingival margins. There was localized supragingival calculus on lower anteriors and generalized subgingival calculus. The treatment plan for this patient included OHI with a power toothbrush, application of Oraqix 2.5% Prilocaine/2.5% Lidocaine for pain management on the first visit and SRP with hand instruments/ ultrasonic scalers. On his second visit instead of Oraqix, 1 carpule of 2% Lidocaine 1:100,000 epi local was used for pain management and the patient responded well. For oral hygiene instructions, power toothbrush is recommended for controlled pressure and effective plaque removal because this patient habitually brushes too hard. As an adjunct to brushing, I also recommended Listerine Antiseptic mouth rinse once a day to manage his Gingivitis. The patient expressed that he learned a lot from what I told him and is compliant with the home care regimen. I advised him to see an Orthodontist if he chooses to remove the mesiodens. Recare for this patient is 6 months.
I choose this case because this patient presents with a mesiodens which caused some anterior crowding and is very sensitive on his maxillary arch. With this finding, it was a challenge for me and I had to modify my treatment. During the first visit, I planned to use only Oraqix topical anesthesia, but I underestimated his pain threshold. However, I was able to make the clinical judgment to use local anesthesia on the second visit as opposed to Oraqix to manage the pain. This patient was also anxious about receiving an injection, I reassured him that he will not feel any discomfort after the injection. Also, I wiggled his lip with a mouth mirror as I gave the anesthesia which distracted him from the injection and it made him more comfortable. After this experience, I felt I had growth in the management of an anxious patient.
Arestin Case:
E. R. 45-year-old Hispanic male presents for dental check-up and prophylaxis. His vitals were BP: 115/89 and pulse: 93. Medical history indicated no systemic conditions, no allergies, and not taking any medications which places him as ASA I. Regarding extraoral/intraoral exam, it was within normal limits. He has class I bilateral occlusion, arrested and filled previously identified caries. Periodontally he presents with generalized 3-4 mm PD with localized 5-6 mm PD on posteriors, recession of 2-3 mm maxillary posteriors, and minimal BUP. Based on these findings, he is diagnosed as Perio type II. Biofilm, stain and calculus detection indicates medium case value. The treatment plan for this patient included OHI with proxabrush where diastema is present such as #2 and #3 due to food getting trapped at those locations. During the same visit, I scaled all quadrants, polished with medium grit prophy paste, and applied 5% fluoride varnish. On the second visit, Arestin was placed on the following areas: #2 ML, #3ML/DL, #4 DL and post-op instructions were given. On the evaluation visit, one month after Arestin placement, only #3 ML and #4 DL showed improvement, #2 and #3 DL probing depths remained the same due to food still getting trapped between those teeth. Therefore, the patient is reinforced to practice using a proxabrush to clean out the diastema after each meal. He understands now that keeping that diastema clean is essential for the recovery after Arestin is placed. Recare for this patient is 3 months.