CASE ONE: Type III Perio Case with Prehypertension
DEMOGRAPHICS
Patient is M.B. Age 60, Heavy / Type III.
ASSESSMENT
Patient has no significant medical history, surgeries or hospital visits. Patient is allergic to cats. His vital signs were significant for prehypertension 141/98 RAS and pulse was 69. ASA II.
Patient is a non-smoker, non-drinker. No pre-medications required. No systemic conditions.
Patient not currently taking any prescription medications or vitamins.
ORAL PATHOLOGY
Patient had 2mm darkened macule on lower left anterior buccal mucosa.
Patient had 4mm white lesion on lower left posterior buccal mucosa.
DENTITION
Patient is missing #1, 16, 17, 20. Retained root tips #31. Porcelain crowns fused to metal #8, 9. Fractured restorations #18. Multiple amalgam restorations throughout.
Class I Occlusion. Overjet: 5mm. Overbite: 90%.
Attrition: #7, 10, 11, 19, 21-30, 32.
Incipient lesions detected #10(L), #11(L), #18(BDO).
PERIODONTAL
Patient had generalized moderate gingival inflammation. Patient had no probing depths exceeding 6mm.
Recession present #6, 7, 12, 13, 20, 21, 27, 28.
Heavy case. Type III. Grade I furcation. Medium extrinsic stain. Minimal bleeding upon probing.
ORAL HYGIENE
Patient’s initial PI Score was 1.3
Patient had subgingival calculus present throughout maxillary and mandibular posterior and anterior regions. Patient had tenacious calculus present on distal surfaces of posterior 2nd and 3rd molars. Patient had supragingival calculus present on facial and lingual surfaces of mandibular anterior teeth.
Flossing was introduced to patient when PI Score was revealed by disclosing agent. I introduced flossing due to interproximal calculus and plaque throughout. In the visit following, PI Score decreased to 1.0 and patient showed success and enthusiasm in improved oral hygiene. Toothbrushing was reviewed at the second visit, where I recommended an electric toothbrush to the patient. This was suggested because of overall need for improved oral hygiene as well as recession. By the third visit, he patient stated they had purchased the electric toothbrush and had noticed improved oral hygiene at home.
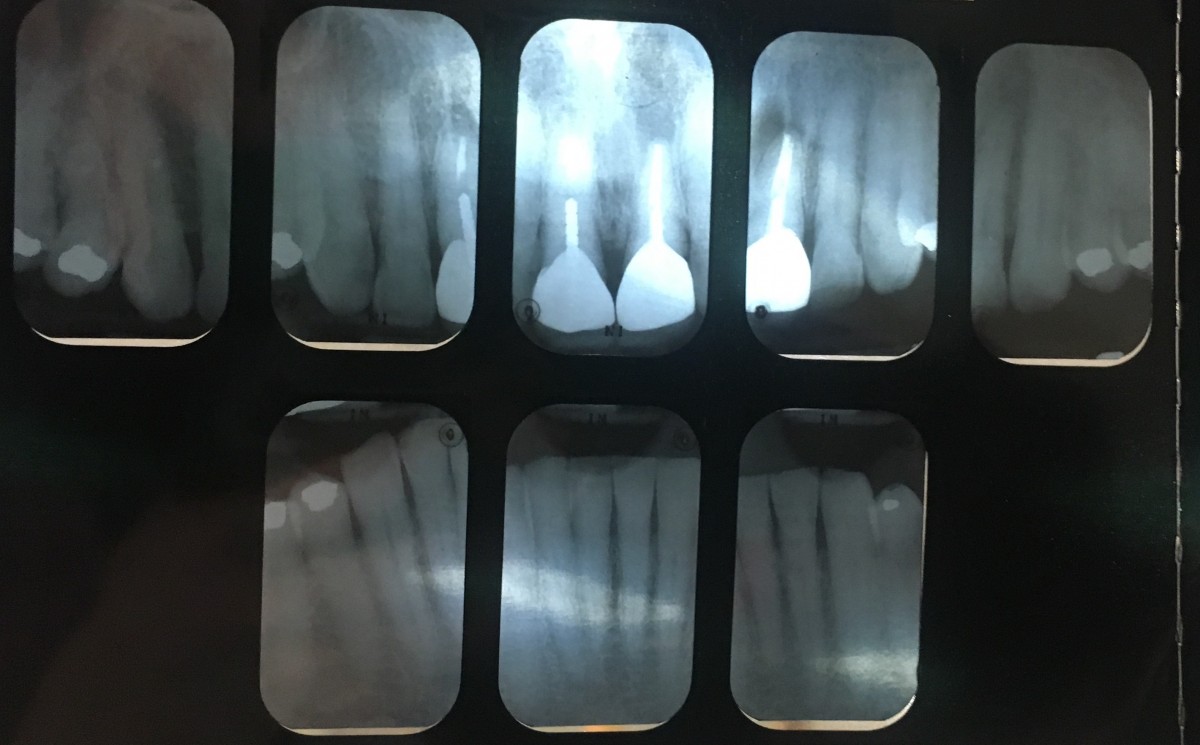
RADIOGRAPHS
FMS was completed 4/22/17 and utilized throughout treatment.
Radiographs reveal a broken post at PFM #8, and PAP at PFM #9.
Radiographs reveal decay in retained root tip of #31.
TREATMENT MANAGEMENT
At the patients initial visit, it was apparent to me that this would be one of the more difficult cases I would have throughout the semester. I know this patient very well, yet never knew the extent of dental treatment that would be necessary. The patients BP was taken twice throughout this visit, as the patient reported not eating earlier that morning, but had 2 espresso’s and one cup of coffee. I do believe this contributed to the high blood pressure reading, as it decreased later on in the visit but still remained a bit high. This patient was referred to a MD to be checked for hypertension regardless. Additionally, this patient was referred to a DDS for caries evaluation, as a fracture was detected in the restoration of tooth #18.
By the second visit, the patient reported an increased use in flossing and had been flossing about every other day. This was an improvement from initially reporting about 1x/week. Patient at this visit reported seeing a MD and had been cleared for treatment. No indication of high blood pressure or use of medication for prehypertension.
An improved PI score of 1 was recorded at this visit, improving from 1.3 about two weeks prior. I did see an improvement in gingival inflammation. The patients improved oral hygiene routine, I do believe contributed to this, in addition to calculus removal. The white lesion detected on the patients lower left buccal mucosa had dissipated by this visit, and upon discussion with the patient, I believe it was a result of cheek biting which the patient had remembered happening earlier in the week. I explained that this could have occurred due to the patients occlusion. The loss of #20 enabled mesial drift of #18 and #19. The position in which they have shifted, I believe, could have contributed to the trauma. I utilized the cavitron and hand scaled. The patient had also reported switching from a manual toothbrush to an electric toothbrush and could not believe the changes it had made in the oral health. It was very rewarding to observe the patients enthusiasm and excitement. At the final visit, the PI score was 1.2. Although it had decreased a bit, I still felt satisfied since it was still better than the initial PI score. I was sure to always review flossing and toothbrushing with the patient. These were the only two aids I had taught the patient, but wanted to implement very little in hopes of the patient focusing just on brushing twice a day, and flossing once a day.
Upon completion of calculus removal, I used a medium prophy-paste to assist in stain removal and applied sodium fluoride foam. The patient seemed very satisfied with both their new smile and the treatment they had received. I was happy to make a difference in this persons attitude toward dental treatment and oral health.
The patient was placed on a 3 month recall due to supragingival as well as very heavy, tenacious subgingival calculus particularly in the posterior sextants.
EVALUATION
The patient was extremely enthusiastic about learning the effects of flossing and the difference an electric toothbrush makes, as compared to a manual toothbrush. The patient seemed to be implementing what was taught because of the improved oral hygiene by the second visit.
The initial PI score was a 1.3 and changed to 1 from beginning to completion of treatment.
The patients gingival tissue decreased from generalized moderate inflammation with bulbous, rolled tissue in the posterior aspects of the mandible to generalized mild inflammation. Although a decrease in generalized inflammation was evident, the consistent detection of residual calculus made it difficult to maintain. I very often had to go back to check for residual calculus, as this was a very heavy case. By the time I had completed the final quadrant (UR), the quadrant I had initially scaled (LL) showed a positive response to treatment. I believe the patients enthusiasm for maintaining a good oral hygiene routine definitely contributed to this improvement.
CASE TWO: Heavy Stain with Partial Denture
DEMOGRAPHICS
Patient is R.S. Age 55, Heavy / Type IV