Case Study #1:
31 year old, Mixed race male who smokes marijuana weekly. BP 148/91 with no current history of hypertension, patient was extremely nervous and BP decreased to 135/80 after an hour. EO/IO was within normal limits. Dental charting: missing #5, #8, #19, fracture on #3L, suspected carious lesion #4, upper partial denture (#8). Perio: generalized 1-6mm pockets, slight-moderate bleeding upon probing, and 1-3mm localized recession. The patient had generalized slight-moderate gingival inflammation, and localized severe gingival inflammation on the linguals of the mandibular anteriors. The patient has denture stomatitis. Calculus: Generalized heavy subgingival calculus, localized supragingival calculus (mandible), and heavy staining (mandible) was present. The patient was a H/II (supported by bone loss evident on FMS). Treatment: I spent time on OHI clearly demonstrating the proper brushing and flossing methods, and explaining denture stomatitis and its prevention. I also recommended using a power brush. I used ultrasonics initially, followed by my hand instruments and then prophy jet. On the revisit, there was substantial reduction in tissue inflammation, supporting the patient’s implementation of proper brushing and flossing. The patient was placed on a 3 month recall.
Calculus, Staining and Inflammed gingiva before treatment.
Gingival tissue Improvement 2 weeks after treatment of right side of mandible.
Completed treatment.
Case Study #2:
22 year old, African American female presents with a history of Asthma (managed with Albuterol as needed), and Multiple Sclerosis (diagnosed 2009). BP 107/72. EO/IO: nasal piercing, tattoo on mucosal lining of lower lip. Dental charting (photos following): several amalgams, PFMs, RCT, recurrent decay and rampant decay (evident on FMS and clinically), several missing teeth, upper partial denture (#6, #7#12). Perio: Localized 4-5mm pockets on the maxillary anteriors and mandiblular molars, and moderate bleeding upon probing. Patient had severe gingival inflammation-red, edematous tissue including papillae with broken marginal gingival tissue on the linguals of #5, #8, #9, #10, #11, due to denture stomatitis. Calculus: generalized subgingival calculus deposits, and localized supragingval calculus deposits on mandibular anterteriors. Patient was a H/I (no bone loss evident on FMS). Treatment: I spent time on OHI clearly demonstrating the proper brushing and flossing methods, and explaining denture stomatitis and its prevention. I also recommended using a power brush. I used ultrasonics initially, followed by my hand instruments, and application of 5% fluoride varnish. On the revisit, there was reduction in tissue inflammation and bleeding, supporting the patient’s implementation of proper brushing and flossing. The patient reported no more bleeding when brushing. The patient was given a referral for rampant decay and was placed on a 3 month recall.
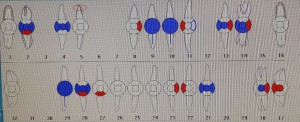
Rampant caries on FMS and dental charting.
Gingival tissue inflammation and denture stomatitis.